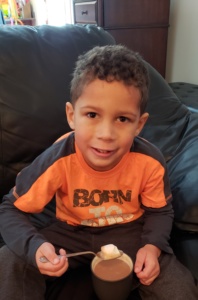
Dylan J | Acidemia propionico | Age 2 1/2
Dylan J was born on October 12th, 2013 in Waconia, Minnesota, weighing in at 8 pounds, 2 ounces. After Dylan was born, the doctors noticed that he had a lower than average body temperature, so they brought him back to the nursery to warm him up. He was brought back to us, and from there on out for two days, we experienced a normal, healthy little boy, or so we thought.
In the early morning hours on October 15th, only 15 hours since we had been discharged from the hospital as a family of 3, Dylan was acting kind of strange. He was very sleepy, and seemed cold to the touch. My husband, Adam, and I took his temperature and he was at 95 degrees. Knowing that wasn’t normal, I called my sister- in- law, who is a NICU nurse here in the cities, and she told us to try doing skin-on-skin to warm him up, and if that didn’t work, to probably call the on-call pediatrician. Much to our dismay, an hour passed and he hadn’t warmed up at all, even after everything we had tried. I called the on-call pediatrician and he told us to watch him over the next several hours, if he was still cold and was still very lethargic and didn’t want to eat, we could wait to bring him to the pediatrician office that opened at 8am that morning, or we could bring him to the emergency room. About an hour later, my husband picked Dylan up to bring him to me to try and feed, and his arms fell limply behind his body. It’s an image that is burned into my mind. We knew at that moment something was wrong, so we packed him up in his car seat and drove him to the emergency room. Once there, they looked him over, and told us that since babies can’t tell us what’s wrong, they would need to do many blood tests and a spinal tap to narrow down what was going on. I remember the ER doctor telling us it was hard to watch little babies get pricked so he told us to go wait in another room (little did I know I would witness far more worse that these pokes in Dylan’s life to come). Dylan’s breathing also started to become extremely labored, he was really trying hard to get each breath in and out. I don’t remember how long we were in the room, but I do remember the doctor coming and telling my husband and I, they didn’t have any results back yet, but they believed he needed to be transferred to a Children’s hospital in downtown Minneapolis, to put him on a ventilator, because he was getting too exhausted from working so hard to breathe. He left the room, and I lost it, a ventilator, for my little baby? What was wrong? Later the doctor came back and said, he actually believed they might be able to just try oxygen, so they were transferring him upstairs, to their NICU, to see if we could get it under control.
It was then, that the waiting game began. They did multiple blood tests, at one point coming to the conclusion that he was just dehydrated. His blood sugar was very low, and they believed he just hadn’t eaten enough. Hours passed by, and we were waiting for the neonatologist that did his rounds around the more suburban hospitals, to arrive and look at Dylan. Around lunch time, the doctor came in and looked at him and told us he believed Dylan still needed to be transferred to the Children’s hospital to be put on a ventilator because the oxygen itself was not cutting it. As he was telling us this, a nurse walked in, handed him a piece of paper, to which he looked at, replied “oh my gosh”, and left the room. We were freaked out, but didn’t think too much of it. Minutes later he came back in and told us that Dylan’s ammonia level was 900. He looked at our very confused faces and told us that this was very, very serious, that the normal range was 10-35, and that Dylan may not make it. I remember being numb, to the idea that my brand new baby could die, when an hour earlier we had just thought he was dehydrated. The doctor left to set up an ambulance to take Dylan, not to the Children’s hospital anymore, but to the University of Minnesota Children’s hospital, because he needed special treatment, only available at the University. He needed to be placed on Dialysis.
I rode in the ambulance with Dylan, and those were the longest 45 minutes of my life. I remember thinking he was going to die in the ambulance, that there was nothing I could do, I just had to sit up in the front seat and pray. Once we arrived at the hospital, it was like a scene out of a movie, all these doctors swarmed us, telling me they’d been waiting, explaining what was going on, needing me to sign consent forms to start dialysis. Telling me that doing dialysis on a 3 day old baby was very risky, but what other choice did we have? By the time we arrived at the hospital his ammonia had climbed to 1200. My husband and I, and our families, were ushered into the family waiting room where we waited to hear word on Dylan. It was at this time we were introduced to our metabolic doctor. She came and met with us and described what she believed Dylan had. A rare genetic disorder, where he could not break down protein correctly, and instead of breaking it down, he would only break down to a certain point and then the bad things (propionic acid and ammonia), would back up in his system. With it being as high as it was, it was poisoning his organs. They told us they believed his brain was swollen and they couldn’t be sure what brain damage he had received from the high ammonia, they would take ultrasounds and an MRI, which both came out fairly good, but really time would tell.
Many hours later, dialysis began, and a nurse came in, and said the words, I will never forget “I know this has been the worst day of your life, but I wanted to give you some good news, Dylan’s ammonia is 90”! As fast as he got sick, he got better just as quickly. They were able to rush Dylan’s newborn screening results and that confirmed his diagnosis of Propionic Acidemia. The doctors now had a diagnosis and were able to treat him. As the days passed in the ICU, his ammonia stabilized, they were able to start him on a low protein diet of Propimex and breast milk, and he did really well. We were able to go home after just 7 days in the ICU.
Life with Dylan after that seemed to go very well, and to us was “normal”. He was a good eater, always ate the amount of protein and calories he needed to get in a day and was developing normally. I would check his ketones in his urine daily (our doctors thought I was a little crazy for checking so much, but it was my indicator something was off), and they were always negative until he was about 5 months old. Dylan started getting trace to small ketones in his urine almost daily. We would try to push more fluids, but they would still go back up. He was eating all of his bottles very well still and acting completely normal. Tuttavia, once we saw ketones, we would bring him in to the emergency room and his ammonia would be high, in the 100’s. The scariest part was, he never acted different, never showed signs his ammonia was high, except for the ketones.
After being in and out of the hospital for weeks at a time between February and May, our metabolic doctors decided to start him on Carbaglu, to help keep his ammonia in check. When we were discharged from the hospital in late April after starting Carbaglu, we met for a follow up appointment with our metabolic doctors. It was at this appointment that Dylan’s doctor sat us down and told us she believed Dylan needed a liver transplant. You see, they were never able to tell us for certain if Dylan had a more severe case of PA or not, because after genetic testing was done, it came back that both of his mutations had never been seen before. So we kind of had to wait and see how he did. We were shocked, never had we thought liver transplant would be something we would be discussing for Dylan. My husband and I went home and for a few weeks thought about it, prayed about it, cried about it, researched it, got stories from other parents that had gone through this, and ultimately decided that we didn’t want to wait until another crisis happened to Dylan and he had brain damage or worse, we wanted Dylan to remain Dylan. So on May 8th of this year, when Dylan was 7 months old, we placed Dylan on the transplant list to get a new liver.
On July 24th, we got the call that they had a new liver for Dylan. We dropped what we were doing and raced to the hospital where they did all the pre-surgery prep work, prepared us, and waited for word as to when the organ would be in Minnesota and when surgery would start. On July 26th, the surgery happened. My husband and I walked Dylan down to the pre-op room and handed him over to the transplant team. We were guided to the family waiting room where we waited with our families for 8 very long hours. When the surgeon came out, with a smile on his face, and told us it had gone very well, it was such a relief. We were taken up to the PICU where we were able to see Dylan, and as scared as I was to see him, when we did, he looked so good. Yes, he was hooked up to so many tubes and lines, and he was swollen, but he looked just like our boy. We stayed in the hospital for 18 days as Dylan recovered. His body accepted the new liver very well, and one of the best moments of our lives, was when our metabolic doctor came in and told us that the organic acid tests they had taken on Dylan after surgery had shown he had no propionic acid in his body! What a miracle.
It’s been almost 2 years since Dylan has had his transplant and he is doing fantastic. He’s had a few complications since but he’s gotten through them with flying colors. Dylan will be on anti-rejection medications his whole life. There’s the fear that he may go into rejection at any time, but if caught early enough, it is very treatable. And here in Minnesota, with our doctors, they will keep a very close eye on him. We also don’t have much research on if this liver will last his whole life, or if he would need a new one eventually, but at the same time, we don’t have a ton of data on what PA does to the body long term. Our metabolic doctors are being very cautious with him, they kept him on his metabolic formula just until this last October when we tried to see what his labs did if he went off it and so far he has remained stable. He is still on a restricted protein diet, right now he gets 30-35g a day. The change in him since transplant has been tenfold. Before he had low tone and now his tone is so much better, he runs and climbs just like every other 2 ½ year old when we’re playing at the park! Anche se era la decisione più difficile che mio marito ed io abbiamo mai fatto, questa è stata la decisione giusta per noi, volevamo Dylan per condurre la vita migliore che poteva, e anche se ci sono stati così tanti rischi, e non sappiamo 100% quello che sarà il futuro, ne valeva la pena, perché è un così felice e molto sano 2 ½ anni ragazzino!